The intentionality of madness: checking the cognitive issues in DSM-based diagnosis
[vc_row][vc_column][ultimate_heading source=”post_title” alignment=”left”][/ultimate_heading][vc_empty_space][/vc_column][/vc_row][vc_row][vc_column][vc_column_text]
 Abstract: In this paper I discuss John Searle’s selective view of intentionality of mental states and place it in the context of impairment to personal identity that occurs in mental illness. I criticize Searle’s view that intentionality characterizes some but not all of mental states; I do so both on principled and on empirical grounds. I then proceed to examine the narrative theory of self, advanced by Paul Ricoeur, Marya Schechtman and others, and explore the extent to which the theory fits a more generalized view of intentionality that would apply to all mental states. This discussion is followed by a brief consideration of the way in which the modern DSM-based psychiatric diagnosis and treatment, reductively and mechanistically, dispense with the issues of ‘strong ontology’, namely the life events and values that mental states might in fact reach for, even when they, on the surface, seem reference-less. In this sense, DSM-inspired psychiatry is based on a Searlian view of mental states. It is contrasted by the narrative theory of self (and therefore also of mental states) which, rather than defining madness by clusters of symptoms, seeks to understand the underlying ontology of reference by looking for both the initial script of the person’s ‘life narrative’ and for ruptures and knots in that narrative that might give rise to madness. Finally I discuss and evaluate the perspective of personality enhancement through counseling aimed at repairing the personal narrative.
Abstract: In this paper I discuss John Searle’s selective view of intentionality of mental states and place it in the context of impairment to personal identity that occurs in mental illness. I criticize Searle’s view that intentionality characterizes some but not all of mental states; I do so both on principled and on empirical grounds. I then proceed to examine the narrative theory of self, advanced by Paul Ricoeur, Marya Schechtman and others, and explore the extent to which the theory fits a more generalized view of intentionality that would apply to all mental states. This discussion is followed by a brief consideration of the way in which the modern DSM-based psychiatric diagnosis and treatment, reductively and mechanistically, dispense with the issues of ‘strong ontology’, namely the life events and values that mental states might in fact reach for, even when they, on the surface, seem reference-less. In this sense, DSM-inspired psychiatry is based on a Searlian view of mental states. It is contrasted by the narrative theory of self (and therefore also of mental states) which, rather than defining madness by clusters of symptoms, seeks to understand the underlying ontology of reference by looking for both the initial script of the person’s ‘life narrative’ and for ruptures and knots in that narrative that might give rise to madness. Finally I discuss and evaluate the perspective of personality enhancement through counseling aimed at repairing the personal narrative.
Key words: intentionality, personality enhancement, counseling, psychotherapy, narrative, script, mental states.
Searle’s view of weak intentionality of mental states
John Searle usefully defines the intentionality of the mind as a general directedness of mental states. Most mental states, Searle says, are intentional not in the sense that they are related to our intentions to do something, but in the sense that they are about the world or concern the world. Mental states generally tend to have a reference outside the mind, although some, admittedly, are self-referential (Searle, 1983).
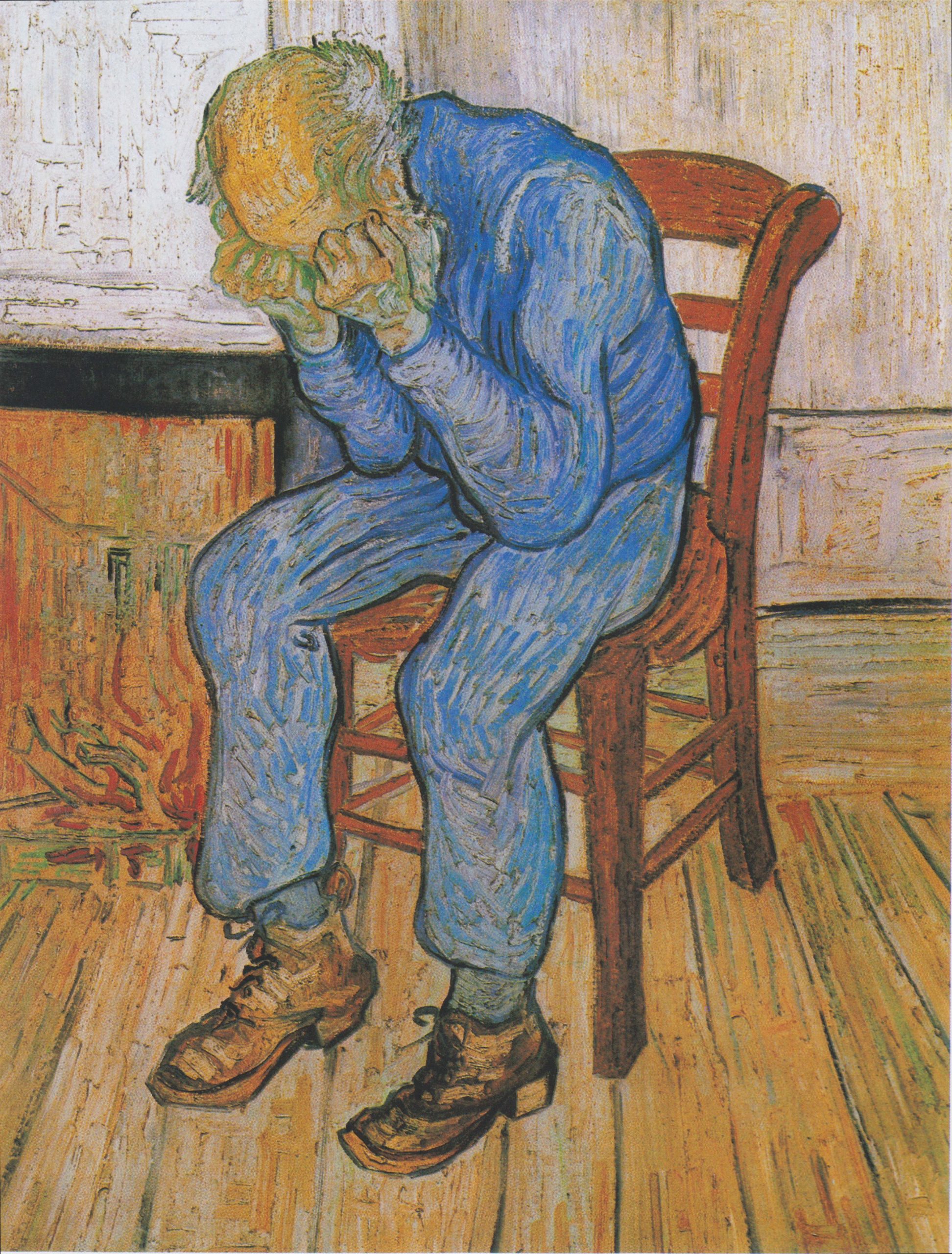
According to Searle there are, however, non-intentional mental states such as elation, depression or anxiety, which appear to be ‘about nothing’. Waking up in the morning and feeling a generalized sense of anxiety is a reference-less mental state on this account, while feeling anxiety about the impending surgery is an intentional mental state. Both instances of anxiety might be characterized by roughly the same emotional content, yet they are different types of anxiety judged by the presence or absence of reference in the outside world (Searle, 1983, p. 2). The mental states that lack outside reference (i.e. non-intentional ones) are distinguished from intentional mental states by being experiences of themselves only (of the feelings that make up the anxiety, depression or euphoria), while intentional mental states are experiences of something outside themselves. This seemingly naïve distinction, which at the time of his writing Searle might have considered a mere remark on the obvious, is constitutive of the main topic of my argument here. The reason is that it generates serious methodological issues for psychiatry and encourages a highly undesirable, reductive understanding of mental disorders and their treatment.
In a nutshell, my issue with Searle’s weak view of intentionality (most mental states tend to be intentional, but some are not) is that there are no sound epistemic grounds for this claim. A person suffering a depressive episode may not be aware that the depression is ‘about’ anything, or that it has a trigger either in the inner experience or in the outside world. It may seem generalized and unprovoked. Trivially, however, the fact that something seems a certain way does not mean that it is that way, especially when this concerns the relationship between mental states and outside events. One may be depressed ‘about’ the general meaninglessness of one’s life and a lack of satisfaction or challenge that has become so familiar that one no longer perceives the clear reference in what appears to be a generalized depression ‘of itself’. Still, this does not make the depression unintentional: all it makes it is appear unintentional to the sufferer. The experience of the sufferer may initially be that of the content of the depression alone, however if pending successful counseling the counselee discovers that the depression was in fact about the general meaninglessness of her life, the experience will become one of depression due to the meaningless of her life, not just of depression of its own. Experiences are not only the prima facie mental states, but also cognitively informed meanings attached to those states. These meanings often include an understanding of the causes of the mental states as integral parts of the experiences associated with such states. The fact that the person may not be aware of the meaning (of which reference is a part) of their mental states does not entail that such meanings do not exist.
On the other hand, a person suffering ‘blues’ because of a romantic break-up accompanied by feelings of intense longing for the lost lover will most likely have a distinct depressive experience ‘of’ the loss she suffered. The two cases may or may not be different types of depression, depending on whether the mental states are actually intentional or not, for which, in Searle, we have no epistemic account at all.
There are many well researched reasons for the blurring of reference in cognitive and emotional states. Notoriously, victims of Post-Traumatic Stress Disorder (PTSD) often blame themselves for their ordeal and suffer protracted periods of depression years after the event where the content of their experience does not appear to refer to the traumatic event at all. Fear and uncertainty often manifest themselves in ‘psycho-somatic’ disorders resulting from long stress that has a clear trigger of which the sufferer is entirely unaware. Various personality crises concerning ‘the meaning of life’ for which people seek counseling often have a seemingly unprovoked onset that, after counseling, proves to have been triggered by a specific dissatisfaction or failure. Examples of only seemingly reference-less states of mania, depression or anxiety are countless.
This concludes the first point I wish to make here: Searle’s weak view of intentionality of mental states is not epistemically sound. There is nothing to prevent us from assuming equally that all mental states are intentional, some obviously so, and some not so obviously. The latter view makes it possible to construe explanations of mental states, and by extension of mental disorders, based on what I will call a ‘strong ontology of referents’, namely events or values whose reality may exert such strong influence on the person that they determine her identity and the fundamental choices she makes to such an extent that, once obscured or blurred, they might precipitate madness. This strong ontology suggests the reality of the good and evil, and the reality of the person’s autonomy to choose one or the other. In this sense, choosing good makes the person good; choosing evil makes the person evil. When the autonomy to make this choice is impaired, when a choice occurs outside the freedom the autonomy creates, or when circumstances blur the very distinction, this can warp the personal narrative so severely that the person becomes ‘mad’. Again, the point is almost trivial in moral philosophy, however in the reductionist psychiatry based on the DSM it is abstracted and represents a major methodological challenge to such psychiatry.
Narrative identity
According to Marya Schechtman and other ‘narrative theorists’, the constitution of a life-story which positions various important events within a single logical context of the past, present and future is the core of personal identity; it allows the formation of continuous self-perceptions and facilitates agency, so that the person is the author of her life (Schechtman, 1996).Disruptions to the personal narrative, or life-story, in times of trauma or identity crises threaten self-understanding and can have a profound influence on our lives, including inducing mental illness.
Schechtman argues that narratives, in order to properly constitute the person’s identity, must meet two key conditions: the articulation condition, and the reality condition. The articulation condition means that the narrative must be sufficiently comprehensible to others and able to explain important events in the person’s life as parts of an ‘intelligible story’ (Schechtman, 1996, p. 114). The reality constraint means that the narrative must be coherent with the basic ‘observational facts and interpretative facts’ (Schechtman, 1996, p. 120). ‘This is because core to being a person is that we engage with other persons and as such we need to agree on the basic features of reality between us.’ (Poltera, 2011, p. 68).
A narrative construction is not simply ‘story-telling’: it is a perspective through which we perceive our lives and define who we are, and it thus must be based on the truth of events and allow for a meaningful interpretation of the past and future plans in order to integrate the personality into an effective agent and ‘owner’ of one’s life. Psychotherapy and counseling are often based on the narrative: once the damaged narrative is restored, ideally the person’s sense of empowerment and functionality will return. At the same time, structures of the narrative are used in counseling to untangle missing references for many seemingly reference-less mental states. Experientially, psychology has arrived at interpretive tools such as compensation, denial or suppression that target precisely the sorts of emotional states that appear resilient to other types of treatment (such as drugs), and may be the result of an ‘unhinging’ of perceptions from their proper reference. Reconstructing the part of the narrative that is missing, blocked or damaged due to various perceptual, cognitive or emotional experiences or problems often re-establishes the basic ‘directedness’, or intentional reach-out of the mental state. Such re-connection to the referent has healing properties in psychotherapy and counseling and is widely accepted as a necessary complement even to pharmacological therapy for psychoses.
The usefulness of the narrative is in its ability to present mental states as communicative states. The pre-requisite for an effective communicative role of the narrative is transparent meaning: at least transparent to the person whose narrative it is. The narrative theory allows us to conceive of mental life as fundamentally communicative, and consequently, of mental issues as ones arising from a distorted or impaired ability to communicate with oneself and with others. The constraints that define a healthy narrative are in fact the pre-requisites for effective communication both on the intra-psychic and on the interpersonal level. Schechtmann correctly identifies two such constraints: a basic consensus on what essential facts define the world that connects us, and a basic consistency and intelligibility of the narrative both within and the narrative and between the narrative and the salient facts of the world. There may be more such constraints, but when the mentioned two are not met, this makes up most official psychiatric diagnoses, from mild neuroses to deep psychoses.
DSM-based diagnosis: The skeptic way
On first glance, the DSM-based diagnosis acknowledges the communicative issues arising from ruptured or warped narrative. It identifies a set of symptoms on various levels and ‘axes’ and provides an algorithm that allows the clinician to ‘calculate’ the diagnosis of mental disorder by simply keying in certain ‘mandatory’ and certain ‘optional’ symptoms and counting each. If the person has x mandatory and z optional symptoms, she is a bipolar, but if one has x-1 mandatory and z+2 optional she is a borderline. If, however, she has x+1 mandatory and z+2 optional she is a bipolar on one axis, and borderline on another axis. If she has x+2 and z+3 she is a bipolar on one axis, and a co-morbid borderline and histrionic personality disorder on another axis, and so on. Each algorithm carries specific prescriptions of treatment, which, seemingly curiously, tends to boil down to just a few generic antipsychotics and a few more mood-modifying drugs that are used across the board of most ‘distinct’ disorders. The discrimination is provided by rhetoric cautions that mention different dosing and a critical role played by ‘the experienced clinician’, however little substance is provided to either convince an informed reader that the classification correlates with any real illnesses, or that there are any real distinctions between many of them, at least on the level of the criteria. This general nature of the DSM is the reason for skepticism about its value as a tool to define and treat mental problems, however it is only a description of what the DSM is here, and is not the primary objection I wish to direct at DSM-inspired psychiatry. Even if the DSM’s classification and method were much more discriminating and precise, the objection I wish to level at it here would hold.
The objection is the following: if epistemological skepticism is expressed in the thesis that ‘we have reason to doubt our knowledge of anything’, then the DSM is a skeptic instrument to interpret mental states. It provides enumerative diagnoses based on collections of mandatory and optional symptoms. The DSM psychiatry does not even consider the meaning of mental issues, nor does it even purport to understand mental states. It is a reductionist approach to mental health that takes mental phenomena at face value without looking for the ontology or the story behind them.
Psychiatrists Thomas Lewis, Fari Amini and Richard Lennan have correctly pointed it out that throughout the 20th century the popular saying was that ‘neurotics build castles in the air, psychotics live in them, and psychiatrists collect the rent’, however it is precisely the psychiatrists and psychologists who spend their time in a castle of theory suspended in the air above nothing (Lewis et al., p. 15). DSM psychiatry believes that it has explained madness by classifying it into diagnoses based on appearances. Just as Bertrand Russell remarked, man is a gullible animal and must believe in something; if one does not have good reasons for such belief, one will belive for bad reasons (as per Lewis et al., p. 17). Instead of seeking to establish whether there are ‘hard realities’ (events and values)that madness is about (other than neurophysiology, which is no more the ontological reference of madness than the mechanics of a car’s engine is the ontological reference of travel), the DSM, in a characteristic reductionist way, does away with intentionality in favour of a seemingly practical functionalism based on collections of symptoms. This turns the quest for the understanding of potential issues of personal identity behind madness into a mere instrumental skill-base for managers of mood and cognition who use drugs. The two vocations are very different indeed, even though, due to the prevalence of psychiatry in the public discourse about madness in the last century, we have become accustomed to this reductionist shift from knowledge to ideology.
The main problem of DSM-inspired psychiatry is, in a sense, in its Searlian reductionism in taking the characteristics of mental states at face value, while forgoing the greater intellectual effort to understand the personal narrative that manifests itself in madness and to relate this understanding to the ‘big’ issues that determine the nature of the persons we are. DSM psychiatry does not ask about reasons for madness, nor does it ask moral questions about the kind of person one is: it shies away from viewing persons in moral terms, medicalising instead many moral concepts and choices. This was well expressed by a psychiatrist whose work with divorcing couples I was able to follow: ‘There are no behavior standards in human relationships; there is no good and no evil. Such distinctions are for priests. In real life, everything is allowed’. This statement was made as a matter-of-fact one, in a counseling session dealing with high moral stakes.
While perhaps more experienced and cautious psychiatrists would avoid making such flagrant nihilistic remarks about the big moral issues involved in personal circles, DSM psychiatry is in fact morally nihilistic in the way well reflected by this unfortunate therapist. Its nihilism arises from its attempt to treat reactions to, or consequences of, morally bad choices as self-sufficient phenomena, and to invent non-moral names even for the most ordinary cases of immoral character. A good example of this ideology of superficiality is the DSM-inspired representation of ‘personality disorders’, which is entirely functionalist in nature. It is well summed up by James Morrison in his practical handbook for psychiatrists to use the DSM IV:
‘All humans (and numerous other species as well) have personality traits. These are well-ingrained ways in which individuals experience, interact with, and think about everything that goes on around them. Personality disorders are collections of traits that have become rigid and work to individuals’ disadvantage, to the point that they impair functioning or cause distress. DSM-IV personality disorders are all patterns of behavior and thinking that have been present since early adult life and have been recognizable in the patient for a long time. Personality disorders are probably dimensional, not categorical. This means that their components (traits) are present in normal people, but are accentuated in those with the disorders in question (Morrison, 2006: 460–461).
Given all the descriptive and conditional statements included in this characterisation of personality disorders, the absence of a strong ontology of reference is quite conspicuous. The diagnosis of disorder morally neutralises bad personality traits: it carefully circumvents the distinction between the ontologically strong ‘good’ and ‘evil’, and allows us to elegantly avoid the question of whether there are people who are simply of bad character, who are attracted to evil rather than the good, who are ill-tempered and unfriendly: in other words, people who make others unhappy.
Throughout human history the distinction between the good and evil marked character evaluations: along with the saints, there were deliberate and habitual sinners; along with heroes ― the traitors, along with exemplary spouses, there were cheats and manipulators, and along with sages there were unreflective and reckless people. The very distinction marks the basic structure of moral autonomy: one is able to choose between the good and evil in most situations; some people will chose the good, the others will opt for the evil. Does the latter choice make them ill or ‘personally disordered’? And if so, what does this do for moral autonomy?
The medicalisation of madness is the easiest to criticize in personality disorders, because they are just so poorly described in the DSM and are treated with such obvious arbitrariness. In most cases it is entirely sufficient for someone to exhibit ‘bad’ personality traits and make evil choices ‘from early adulthood’ to be diagnosed with a personality disorder, depending on the specific nature of the ‘badness’ of character that one chooses.(or acquires). However the deeper philosophical failure of DSM psychiatry here is the same as with its interpretation of mental states generally: although psychological theories ascribe a degree of freedom of choice to people who develop various mental health problems, the general approach to such problems after their onset is to deprive them of reference and, by extension, of intentionality, and ‘manage’ them’ as self-sufficient phenomena.
Transactional analysis, for example, insists that a young child ‘decides’ to adopt a certain ‘life script’ in response to certain typical situations that the child encounters, although such reaction is by no means necessary, and not all children will adopt the same script. The outcomes that the script may lead to and often do include madness or suicide at a later stage in life. Regardless of the epistemological foundations of such claims (or the similar yet even more epistemologically problematic claims of psychoanalysis), which, upon careful analysis, turn out to presume everything and prove nothing, the assumption of freedom of choice is built into the foundations of most psychological theories of the origin of madness. This freedom is cancelled out by the DSM-based diagnosis and treatment: even the psychotherapy that is administered after a DSM diagnosis tends to be manipulative rather than truly discursive, and treats the ‘patient’ as a means, and not as an end in oneself: it completely cancels out the presumption of autonomy. In its reductionism, the DSM psychiatry thus militates even against the psychological theories that parented it as a discipline.
The DSM-based approach is cognitively self-limiting and philosophically skeptical, because its methodology does not envision the possibility of understanding madness or mental states in general as meaningful and based on a set of hard realities (including the big values) of life that the illness might be a conceptualization or projection of, or a reaction to. The DSM does not deny such hard realities or the intentionality of madness as such; it merely assumes that there is no way of knowing or proving such intentionality, and therefore, in the standard skeptic manner, reduces the concept of madness to collections of symptoms; correspondingly it reduces healing madness to the management of symptoms.
The perspective of therapeutic personality enhancement
Just as a person is more than a collection of character traits, so a mental state is more than a set of its symptoms. There seems to be little principled argument against the idea that healing madness, if it was possible, would have to include healing the person rather than managing the symptoms; however the skeptic approach taken by western psychiatry nicely converges with Searle’s (and others’) reductionist view of mental states as either intentional or unintentional depending on whether they have an obvious referent outside the immediate experience itself. Contrary to this approach to mental life, the narrative theory acknowledges the possibility (and likelihood) that all mental states could have an essential reference and might thus be essentially intentional, whether this is obvious (as it is in examples given for intentional mental states by Searle), or less so (the extreme being many cases of madness). The narrative theory is cognitively optimistic, and envisions the possibility of addressing mental issues at their root by seeking to understand its intentionality. It does not deny the neurophysiological aspects of madness, nor does it claim, in its mainstream form, that psychiatric treatment is not necessary. To the contrary, psychiatric treatment is absolutely necessary for most mental health patients, however it is not sufficient either to understand, or to heal mental problems; it supervenes, as it were, on a more fundamental and more holistic view of the person, the suffering and the spirit involved in and affected by mental disorders.
For all of the above reasons, it seems to me that curing mental illness is inseparable from personality enhancement. In fact, nothing short of working on repairing the narrative, with the concomitant full recognition of its missing reference and a comprehension of the intentionality of mental life as a whole, may amount to curing madness, no more than mere cardiac surgery to by-pass the blocked blood vessel is sufficient for achieving holistic vascular health. The phrase ‘therapeutic personality enhancement’ thus seems warranted; it is capable of integrative psychopharmacological intervention, when necessary (and admittedly it is often necessary), the managerial approach to mental health that characterizes psychiatry, and the deeper and further-reaching methodology of work on personality enhancement through repairs and enrichment of the life narrative, or personal identity. In this perspective, madness is a problem of identity and autonomy, both of which are closely inter-related.
Counseling and psychotherapy are geared to improving the quality of life by enhancing the strength of personality and helping people adapt their value systems and emotional reactions to the reality that they share with important others. Philosophical counseling in particular can help people ‘appraise the pragmatism of their personal values and sentiments, and thereby help to buffer them against their emotional whims. This model is not “therapeutic” in the sense of healing mental illness, but it aims to improve the quality of life’ (Brown, 2010: 112). Some philosophical counselors, such as Peter Raabe, go a step further and argue that philosophical counseling is a form of therapy even from clients suffering from serious mental disturbances: ‘(…) philosophical counseling is an attempt to both understand and alleviate the suffering of another human being’ (Raabe, 2002: 98). Raabe in fact goes as far as saying that psychiatric diagnoses are more or less arbitrary labels, and that psychotropic medication generally does not work, saying specifically that ‘it is a placebo’ (Raabe, 2009: 95-97).Whatever the merits of those arguments, clearly counseling in all its forms is aimed at facilitating the human flourishing by removing anguish and emotional problems via facilitating the acquisition of explanatory insights.
Conclusion
Searle’s selective intentionality thesis addresses mental states in healthy people, and suggests that there are reference-less ‘elation anxiety or depression’ just as there are elation, anxiety and depression that are clearly intentional. The rich experience of psychotherapy and counseling in their various forms shows that in many cases of seemingly unintentional mental states in healthy people the uncovering of a reference, and thus the restoration of the sense of intentionality of these states, has led to personality and/or mood improvement. Thus, it seems, there is no more reason for the selective intentionality thesis than there is for a ‘full intentionality thesis’, namely the thesis that all mental states at least in healthy people are intentional. Arguing this does not prevent us from allowing, unlike Raabe, that there is indeed genuine mental illness which requires medication, without prejudicing the claim that the mental states of mentally ill people may also be universally intentional, though admittedly more severely obscured than those of mentally healthy individuals. This idea seems supported by the experiential fact that mental illness is often precipitated by ‘triggers’: many mentally ill people appear (and perhaps are) ‘normal’ for much of the time; only in certain particularly provocative situations (provocative for them, not necessarily to be seen as such by others) does their illness flare up and they exhibit clear signs of mental disorder. This would suggest that their mental life is also fully intentional, directed to and concerned about the external world, namely that it crucially strives towards an ontologically strong referent. If so, their illness might largely arise from the denial of transparent reference. This obscurity might block the self-communication power of the personal narrative thus threatening their sense of identity and, consequently, disrupting their mood and ability to govern themselves so severely that they enter the realm labeled ‘madness’. By extension, they enter the management game of DSM psychiatry which, by its reductionist myopia and lack of interpretative courage, promises to treat their symptoms as ‘reference-less’, non-intentional mental events whose ontology does not go beyond the chemical, electrical or anatomical realities of their brains.
Author: Aleksandar Fatić
References:
Brison, S. (1997), Outliving Oneself: Trauma, Memory and Personal Identity. In D. Meyers (ed.), Feminists Rethink the Self, Colorado, Westview Press, pp. 12-39.
Brison, S. (2002).Aftermath: Violence and the Remaking of a Self. Princeton: Princeton University Press.
Bruner, J. (2003). Self-Making Narratives. In R. Fivush and C. Haden (eds.), Auto-biographical Memory and the Construction of a Narrative Self: Developmental and Cultural Perspectives, pp. 209–226. New Jersey: Lawrence Erlbaum Associates.
Dennett, D. (1992). The Self as a Centre of Narrative Gravity. In F. Kessel, P. Cole, and D. Johnson (eds.), Self and Consciousness: Multiple Perspectives, pp.103–115. New Jersey: Lawrence Erlbaum Associates.
Hutto, D. (ed.) (2007). Narrative and Understanding Persons. Cambridge: Cambridge University Press.
Kircher, T. and David, A. (eds.), (2003).The Self in Neuroscience and Psychiatry. Cambridge: Cambridge University Press.
Lewis, T. et al. (2009). A General Theory of Love ― Croatian translation: Opšta teorija ljubavi, translated by Mirna Vilišić. Zagreb: Profil.
Morrison, J (2006). DSM-IV Made Easy: The Clinician’s Guide to Diagnosis. New York: The Guilford Press.
Nelson, H.L. (2001). Damaged Identities, Narrative Repair. New York: Cornell University Press.
Poltera, J. (2011). Self-Narratives, Story-Telling and Empathetic Listeners.Practical Philosophy 10, 1: 65-79. (web edition).
Raabe, P. (2002). Issues in Philosophical Counseling. New York. Praeger.
Raabe, P. (2009). ‘Philosophy in a Psycho-Pharmaceutical World’, Practical Philosophy 9,2: 95–97.
Ricoeur, P. (1991). Narrative Identity. In D. Wood (ed.), On Paul Ricoeur: Narrative and Interpretation, pp.188–199. London: Routledge.
Rudd, A. (2009).In Defence of Narrative. European Journal of Philosophy 17(1):60–75.
Schechtman, M. (1996).The Constitution of Selves. New York: Cornell University Press.
Searle, John (1983), Intentionality, Cambridge, Cambridge University Press.
Strawson, G. (2004). Against Narrativity.Ratio (new series) XVII: 428–452.
Taylor, C. (1989). Sources of the Self. Cambridge: Cambridge University Press.
Wells, L.A. (2003). Discontinuity in Personal Narrative: Some perspectives of Patients. Philosophy, Psychiatry and Psychology10(4): 297–303.
Wollheim, R. (1984). The Thread of Life. Cambridge: Cambridge University Press.
Woody, M.J. (2004). When Narrative Fails. Philosophy, Psychiatry and Psychology, 10(4): 329–345.
[/vc_column_text][/vc_column][/vc_row]